March 29, 2018 – Every five years I go through the prep for a colonoscopy. It involves drinking a vile mix of laxatives to clean out my intestines over two days prior to the procedure. Then I submit myself to a scoping of my large intestine. I do this because twelve years ago polyps were discovered in my intestine. The biopsy of these polyps showed they were non-cancerous. But my gastroenterologist told me that it would be in my best interest to repeat the test every five years until no polyps were detected. So far each new colonoscopy procedure has led to the discovery of more polyps.
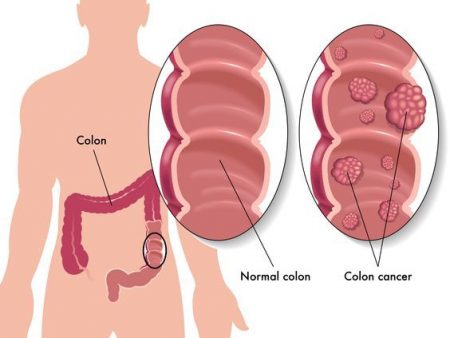
I am far from alone in having to go through this cycle of repeat testing. Colorectal cancer (CRC) is the third most common cancer in humans. As our global population ages CRC is expected to increase by 60% to 2.2 million new cases annually by 2030, and 1.1 million deaths.
Yet CRC which occurs in men and women more often after age 50 is preventable through regular screening which can find pre-cancerous polyps and remove them before they become cancer.
And since CRC is asymptomatic in its early stages, without screening you may never know you already have it.
Is a colonoscopy the only screening method to detect CRC?
There are other means by which CRC can be detected. These include:
- Sigmoidoscopy
- Barium enema
- CT colonoscopy
- Fecal occult blood test
- DNA fecal test
But the gold standard remains the colonoscopy which involves inserting through the rectum and into the large intestine, a flexible tube called a colonoscope. The tube contains a video camera and light, and instrument port to allow the colonoscopist to use a tool for excising and sampling suspect tissue. Images are viewed on an external monitor.
Making colonoscopies smarter
Finding pre-cancerous polyps, called adenomas, and literally nipping them in the bud is today the best way to stop CRC before it starts. But colonoscopies don’t catch every adenoma. In fact, the rate of detection varies from 7 to 53% based on the skills of the colonoscopist. The best in the business may get to 80% detection rates during and in post-procedural review.
Increasing detection by 1% is a big deal because it reduces the risk of CRC by 3 to 6% within 5 years of having a colonoscopy. That’s why the researchers at UC Irvine are applying artificial intelligence (AI) algorithms to see if they can increase adenoma detection rates and eventually have the tool identify cancerous ones on the fly.
Dr. William E. Karnes is the team leader in the research. He is working with UC Irvine Health, and AI specialists at DocBot, a university AI spinoff. So far the algorithms developed by DocBot are encouraging, finding far more adenomas than the best of UC Irvine’s high-risk colon cancer colonoscopists. Karnes describes the first results, applying the tool to review video feeds from past colonoscopies.
“We had them [the colonoscopists] mark every polyp they saw. On first review, they found about 20% more polyps than the original colonoscopist had removed. Then they viewed it with an AI overlay; AI found all the polyps they had discovered, plus about 20% more.”
And the AI tool processes 98 images per second, four times faster than the live video feed from a colonoscopy procedure. But now comes the important next step: starting to use the tool during live colonoscopies to see, if in real-time, it can increase rates of polyp detection and provide warnings to the colonoscopists during the procedure.
What Karnes hopes will be the final product is a tool that will not only identify adenomas but also detect whether they are benign or cancerous in real time. That could increase detection rates to a point where virtually no adenoma gets are missed and CRC is caught at its earliest stages before it can progress.