Is drug addiction a disease? It may start with a voluntary sampling of a cigarette, an amphetamine, a stimulant, a depressant….but what eventually happens is in fact a dependency driven by our brains. We continue to use the drug for its effect even though it adversely affects our lives. Addictive substances impact the brain’s frontal cortex. That’s the area of our brain that governs decision-making and judgment. Addiction acts like a runaway train by interrupting the normal brain circuitry making the craving for whatever the substance is overwhelming.
Is everyone susceptible to addiction? It’s a good question because environment may be a strong determining factor.
What motivates someone to try an addictive substance? Often it’s curiosity. Other times it’s stress brought about by circumstances. Sometimes it’s peer pressure, a wish to be a part of a social group, sharing something in common. So circumstances play a role in susceptibility.
What makes an addictive drug work?
Why does our body accept this type of foreign substance?
The chemical structure of most addictive drugs mimics brain chemistry fooling our neurons and in particular neural receptors.
Let’s look at marijuana as an example.
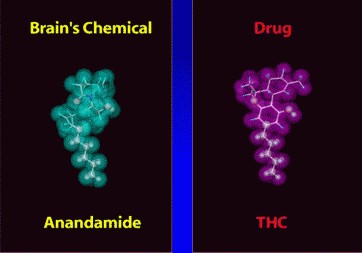
The active chemical in marijuana is THC (tetrahydrocannibol). As you can see from the illustration above THC (on right) is a fairly complex molecule. It is fat-soluble allowing it to slip through the barrier that isolates the brain from the rest of our body systems. THC binds with a neural receptor that is the same one used by a naturally occurring molecule, Anandamide (the molecule on the left).
First identified in 1992, Anandamide was discovered by Dr. William Devane at University of Wisconsin, and Dr. Raphael Mechoulam, at Hebrew University of Jerusalem. Synthesized in an area of the brain that governs memory, higher thought processes and body movement, the two researchers named it after the Sanskrit word that means bliss. Why? Because in finding Anandamide these researchers were identifying the natural human-generated equivalent to THC, a chemical that regulates pain, appetite, mood and short-term memory in the brain.
How do Addictive Drugs Interact with Our Brains?
Neural receptors are the key to nerve cell communication. Chemicals that mimic those naturally produced need a way to take part in that communication. In the example we have looked at THC versus Anandamide, the former binds with receptors on the surface of nerve cells in the same way as the latter.
Anandamide is a “key” molecule because it unlocks a cell by binding with receptors on the cell surface. It does this because its shape fits the receptor like a key entering a lock. When it interacts a door opens through the cell membrane causing a flood of chemicals to enter the nerve cell affecting its positive or negative charge.
THC does exactly the same thing because its shape can also bind with the neuron receptor. The difference in the body response to THC versus Anandamide is one of duration. Where Anandamide is fragile and very short-lived, THC is far more robust. So the bliss effect of Anandamide is short-lived, where the bliss effect of THC can go on for a long time producing the perpetual “high” associated with smoking marijuana.
Most of the drugs we use for pain management work in a similar way. Morphine locks into an opiate receptor in nerve cells. Its natural molecular equivalent is enkephalin. Morphine is addictive because when it binds with a nerve cell receptor it locks even tighter than enkephalin and remains attached. Pharmaceutical companies recognized the addictive nature of morphine and developed less potent substitutes like codeine and demerol.
Addictive drugs elevate another brain-synthesized molecular chemical, dopamine. Dopamine acts like adrenaline affecting the brain processes that govern emotional response, pleasure, pain and body movement. Excessive dopamine creates brain euphoria. Drugs that induce strong dopamine responses are called dopamine agonists. Cocaine is one of these. It binds with the dopamine receptor on the surface of a neuron inducing an excessive dopamine response.
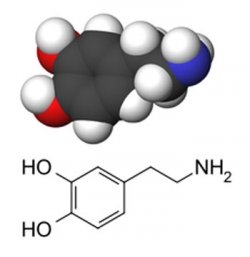
Over time neurons exposed to drugs like cocaine and amphetamines become desensitized or tolerant to dopamine. In these cases each exposure produces less of drug response. The neurons, in anticipation of the drug, stay in a state of stimulation requiring more to create the same effect. How cocaine does this is by binding and hanging on to the proteins that transport dopamine and remaining longer elevating the dopamine response. Amphetamines work similarly leading to over stimulation of the neurons.
Is There an Addiction Vaccine in the Near Future?
Traditional treatments for addiction have involved finding a less addictive drug such as methadone to help reduce heroin dependency, or using a nicotine patch to help stop smoking. Another drug, Vivitrol, has been used to treat alcoholism and opium addiction. There are even anti-smoking pills that don’t act as drug mimics but instead inhibit the neural receptors.
A vaccine approach pursued since the 1970s, has only recently been able to see dramatic progress in creating cocaine immunity. Dr. Ronald Crystal, at Weill Cornell Medical College, has led a team that has produced a vaccine to treat cocaine addiction.
The vaccine was created from a modified version of the adenovirus, the virus for the common cold, discarding the content that causes colds and using the remainder as a carrier medium. A molecule constructed to resemble cocaine is injected into the adenovirus and when a human is vaccinated results in an immune system response. The reason for using the adenovirus is simple. Most addictive drugs are too small for detection by the immune system which allows them to get by the body’s defences. By combining the synthesized drug molecules with a carrier already recognized as pathogen, the immune system learns to attack the smaller drug molecules as pathogens as well so they never reach the neural receptors of the brain. In laboratory tests the vaccine’s effect lasted more than 13 weeks causing an immune response anytime mice “snorted” cocaine.
A similar medical project has used a modified cholera bacteria as a transport mechanism with cocaine creating an immune system response to produce antibodies. In 2009 Baylor College of Medicine in Houston ran clinical trials using this cholera-based anti-addiction cocaine vaccine with 115 human subjects. The results showed a strong antibody response in 38% of patients who received the vaccine, and 45% of remained cocaine free in follow-up examinations up to 4 months after. The vaccine is currently in national clinical trials in the United States. Eventually vaccines of this type could be delivered regularly much the way some people take allergy shots, continually boosting the immune response and eliminating the negative body responses to cocaine ingestion.
Recent researchers at The Scripps Research Institute have had successful results developing a similar vaccine for heroin addiction and have tested it in animal models.
Research into vaccines focused on treating smokers for nicotine addiction is on the way. But alcoholism, the most prevalent addiction, remains untreatable through vaccination.
Considering the cost society bears to deal with addiction, policing the illegal drug trade. and the cost of incarceration for repeat drug dealers and offenders, anti-addiction vaccinations represent a better future.