If your heart fails today you have a number of medical choices. These include:
- using pharmaceutical aids that can prolong the functioning of a failing heart for a significant period of time;
- getting a device implant to boost the functioning of a deteriorating heart;
- replacing the heart with a mechanical device, or:
- receiving a human heart transplant.
But donor demand far exceeds supply with only 4,000 hearts available for more than 100,000 on wait lists. That’s why artificial hearts, mechanical devices that mimic the heart’s beat, are being developed to act as bridging devices to extend a patient’s life until a heart becomes available. And in some cases manufacturers are hoping to develop devices that can replace the natural heart entirely.
One of these companies is SynCardia Systems, located in Tucson, Arizona. It has built an artificial heart that today is implanted in more than 1,100 human patients accounting for more than 300 patient-years of use. The SynCardia artificial heart combines an implant, seen below, with an external control system that the patient wears. Tubes are inserted through the skin. The tubes pump air into two small balloons which then push blood through the implant to the circulatory system. SynCardia is not meant to be a permanent replacement for a real heart. But it does give patients some freedom from hospitalization while waiting for a transplant. In 2012 the Federal Drug Administration in the United States approved SynCardia as a bridging device. The company’s ultimate goal is to have future version of the device approved for permanent use in cases where patients are not transplant eligible. Currently the biggest drawback to the SynCardia implant is the 6 kilogram (13.5 pound) portable, wearable power supply that constantly needs recharging every 4 to 6 hours.
Carmat, a Paris-based company, hopes to improve on all aspects of the SynCardia solution. Its artificial heart combines biology with mechanical components. A membrane made from a cow’s pericardium (the tissue that surrounds the heart) separates the moving parts from the blood system minimizing the need for the patient to be on anti-coagulants. The Carmat is truly a biomimetic device. It looks a little bit like a heart (see the picture below) and its valves are made from biological tissue. In addition it uses 12-hour rechargeable lithium-ion batteries weighing 3 kilograms (6.6 pounds) to power its two artificial pumping chambers, each filled with hydraulic fluid, not air. This means no large tubal inserts through the skin into the body. It is the movement of the fluid between the pumping chambers that mimics the natural heart while never interacting with blood. And Carmat plans to replace its current battery pack with a portable fuel cell making the system the first to use such a power supply in a medical device.
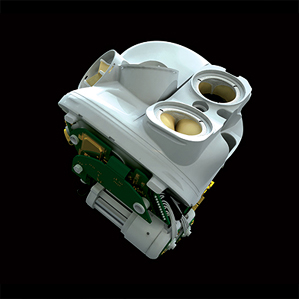
But SynCardia and Carmat are not alone. Last year I wrote about the HeartMate II, a left-ventricle assist device that has been implanted in thousands around the world. And an Australian biomedical engineer, Daniel Timms, has teemed up with the doctors at the Texas Heart Institute to develop an artificial heart that doesn’t beat. Called the BiVACOR artificial heart, it uses a magnetic field, centrifugal force and a single moving part, a spinning disc, to push blood through the body. The prototype can be seen in the picture below. It is hoped by the medical team at the Texas Heart Institute that they can begin human medical trials in a few years.