April 29, 2017 – In Part 1 of this series on the God Cell I introduced the term stem cell and its origins and went on to describe embryonic stem cells and how they are harvested and cultured from fertilized, denucleated embryos.
In this posting, I will talk about what makes stem cells tick? How do they go from being unspecialized cells to become specialized?
As scientists have learned more about stem cells they have also found out that they can be found in every tissue type in our bodies. In the past, they were overlooked because they would show up when looking at a slide of muscle tissue, bone, or lymph nodes, as small and innocuous cells with no known purpose. With hundreds of different cell types performing totally different body functions, cells that didn’t seem to do anything just didn’t ring any bells.
Our first discovery of stem cells came from studying embryos. Embryos begin as a ball of undifferentiated cells, the product of the initial division of a fertilized egg. But early on these undifferentiated cells take on specific tasks and eventually differentiate into hundreds of cell types. From first identifying the differentiating capability of embryonic stem cells, science soon moved on to discover stem cells elsewhere: in amniotic fluid, umbilical cord blood, and bone marrow.
One of the differentiated cells that come from stem cell precursors forms connective tissue. It is known as a stromal cell and is found in bone marrow, lymph nodes, ovaries, uterus, and prostate gland. Stromal cells come in two types: fibroblasts and pericytes.
Fibroblasts form connective tissue. They synthesize collagen which is responsible for providing the framework for various body tissue types.
Pericytes are the cells that help to form the superstructure for blood and lymph vessels.
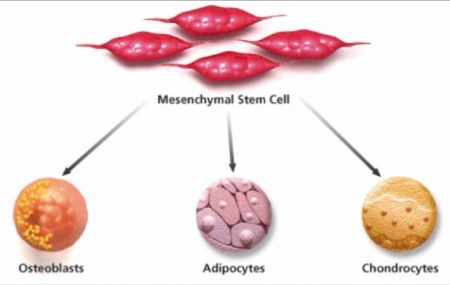
Other types of body cells include a group of four with a common stem cell origin. These are osteoblasts which make up our bones, chondrocytes, our cartilage, myocytes, our muscles, and adipocytes, our body fat. Their common stem cell is referred to as mesenchymal (see illustration below).
Mesenchymal stem cells (MSCs) are one of three types of stem cells responsible for building all the pieces that make us. MSC is to connective tissue as hematopoietic is to red and white blood cells, and platelets and endothelial is to blood and lymph vessels. The process that activates differentiation makes all of these three adult categories of stem cells produce differentiated organelles of various shapes, size, and featuring very different metabolic functions.
So what makes differentiation happen?
DNA, the essential molecule of life contains a blueprint of who we are going to be. It is found in genes on chromosomes forming the nucleus within our body’s cells. The DNA, RNA, and proteins within the cell all work in partnership. The DNA in the genes contains the bodybuilding instructions. The RNA and specific proteins execute the plan.
All this we understand. But we still don’t know the trigger that induces differentiation.
We can see it happen when we harvest stem cells and then inject them into an area in our body where they immediately begin to differentiate into the type of cells found there.
This is the state of regenerative medicine today.
Having said that we’ll conclude Part 2. In our next posting in this series, I will delve more deeply into the use of mesenchymal stem cells in therapeutic application. I’ll describe how these cells are harvested and the current technologies available to us. And I’ll also talk about current clinical trials where mesenchymal stem cells are being used for therapeutic regenerative medical treatment.