February 9, 2018 – Our daughter was born with heart-lung disease and from her birth until today we have been vigilant in getting the flu vaccine every year. That along with precautions such as washing our hands after being outside, using hand sanitizer when out, and keeping our gloves on when in crowded buses and subways, we have managed to not catch the flu for 34 years. Getting the shot has never created any reactions other than mild arm soreness at the site of the injection. That didn’t even happen this fall when we went for our vaccination.
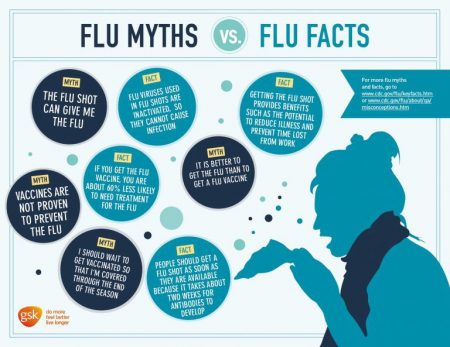
But the antivaccine movement leaves no myth untold when it comes to vaccines including the one for the flu. The result is less than 60% of children, and just over 40% of adults in the United States bother to get vaccinated even though most have coverage through government or private insurance. In Canada, the statistics are not too dissimilar even though the vaccine is free to all.
Here are some of the antivaccine myths we continue to hear.
- Flu isn’t dangerous. Tell that to the more than 100 who have already succumbed to the disease in the United States so far this season. The truth is children and seniors are vulnerable, as are people with existing respiratory or heart conditions.
- You can get the flu from the flu vaccine. This is the greatest myth of all. At most you may get a mild flu-like reaction that lasts for 24 hours before dissipating.
- The vaccine is incubated in chicken eggs and if you have an allergy you shouldn’t get it. But current methods of creating the vaccine have eliminated this issue.
- If pregnant you could give the flu to your fetus. This is another major myth. In fact, the vaccine improves both fetal and maternal outcomes by lessening the likelihood of the latter getting the flu and giving it to the yet-to-be-born child.
- The current vaccine is only 10% effective so why bother to get it. An explanation of just how incorrect this statistic is follows.
What’s In the Current Vaccine
It contains antigens for 4 flu virus:
- Type A H1N1
- Type A H3N2
- Type B/Phuket/3073/2013–like virus
- Type B/Brisbane/60/2008–like virus.
Against 1, 3, and 4, the vaccine is proving to be highly effective. The Center for Disease Control rates it at 70% against the Type Bs, and 60% against the Type A H1N1. The effectiveness against Type A H3N2, however, has proven to be around 30%. So even where it is less effective it is three times better than the 10% myth.
Since vaccines are formulated as much as six months ahead of an outbreak, scientists pick the strains that erupt in the Southern Hemisphere to determine what the composition is for the Northern Hemisphere. That’s because when winter flu season is happening south of the equator, it is summer in the north when flu is seldom seen.
The problem with Type A H3N2 this year is its rate of mutation during its incubation in preparing the vaccine. That means what scientists produced in the formulation did not synch up with the active strain of the virus circulating in the general population. It had already mutated. Hence a 30% effectiveness rate.
This is further complicated by the fact that the previous year’s vaccine suffered from the same problem leaving people at risk to Type A H3N2 two years running.
New methods for incubating future flu vaccines may help overcome the rapid mutation issue.
So if you still haven’t had the flu vaccine this year, at the halfway point of the season, it still makes sense to get it because, with the exception of the Type A H3N2, coverage is highly effective. And even for the H3N2, 30% effectiveness is better than zero protection.