|
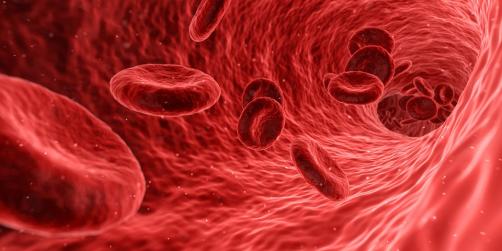
About fifteen years ago bloodwork ordered by my family doctor indicated my cholesterol levels were a little above high normal. My doctor prescribed a statin which I continue to take a minimal dose each day. It took awhile for me to adjust to a side effect – lower back pain, but by adding CoQ10 to my daily intake I have had no problems. High cholesterol levels in the blood are a potential heart disease threat because an excess can cause fatty deposits to grow on the walls of blood vessels which over time can lead to blockages, a stroke, or a heart attack. High cholesterol can be an inherited condition. It can also occur from an unhealthy diet, other medications, or a lack of exercise. The prevalence of high cholesterol in North American populations has had some in the medical profession suggesting that statins should be added to the drinking water, just like fluoride used to prevent tooth decay. Cholesterol in combination with proteins expressed through genetic instructions produces a substance called lipoproteins. There are two versions: low-density lipoprotein (LDL) and high-density lipoprotein (HDL). It is LDL that causes fatty deposits. HDL is seen as good because it removes excess cholesterol from the bloodstream. Taking statins targets LDL and in some studies is seen as increasing HDL levels in blood plasma. But it is still unclear whether statins impact HDL effectiveness. But what if we didn’t need statins and could end high cholesterol by altering a specific gene associated with blood cholesterol levels? In Peter Diamandis’ latest musings he describes what appears to be a biomedical game changer. A therapy that permanently alters one gene responsible for a protein that produces LDL and HDL. I have edited Peter’s work and hope you find what follows to be an interesting read. Heart disease accounts for roughly 16% of total deaths globally each year. It costs the US economy roughly $219 billion annually. High levels of cholesterol in the bloodstream is one of the main causes. That’s why more than 200 million people worldwide regularly take statins, the leading medication for lowering cholesterol levels. These drugs have proved effective, but require consistent use and can result in side-effects. Scientists have identified a link between the PCSK9 gene and a protein for which it is responsible that plays a role in regulating cholesterol levels in the blood. PCSK9 and Heart HealthResearch at the University of Texas Southwestern Medical Center in the mid-2000s established the role of the PCSK9 gene in heart health. The researchers identified people with a genetic mutation that inhibited it from producing a protein had lower LDL levels in their bloodstreams. The PCSK9 gene-produced protein was seen as preventing the recycling of receptors in the liver responsible for filtering LDL from the bloodstream. Where the PCSK9 gene produced high levels of the protein the overall number of receptors dropped and cholesterol levels rose. The impact of the amount of protein produced by the PCSK9 gene was associated with 15 to 28% reductions in LDL levels and a 47 to 88% lower risk of heart disease. Finding a drug that could target the protein has proven challenging. Monoclonal antibodies that target PCSK9 called alirocumab and evolocumab have been produced to cut the risk of cardiovascular events by half. But these drugs are more expensive than statins. CRISPR Edit of PCSK9 = CureThe Texas Southwestern researchers thought that a more promising approach would be to tackle the errant gene rather than the protein it produces. From the patients they identified that had mutations and low LDL levels, it seemed possible to genetically replicate a resistance to heart disease by changing all PCSK9 genes to express less protein. The tool of choice for this project was CRISPR. The emergence of the CRISPR-Cas9 system has revolutionized our ability to tweak genes. There are issues however that have limited its applicability in biomedicine. That’s because the Cas9 protein produced by CRISPR cuts both strands of DNA at a target site before relying on the cell’s internal repair system to stitch the DNA together. Experience has shown that the process isn’t always perfect leading to unintended edits that reduce efficacy and can potentially introduce harmful mutations. An emerging approach known as base editing gets around the problem by using a modified Cas9 protein to break only one of the DNA strands. This is spliced to another protein to convert one DNA letter to another. The approach only makes single letter edits but is much more precise for use in medical applications. And by a remarkable stroke of luck, it turns out that the PCSK9 gene can be altered to deal with the errant protein through a simple one-letter edit. This is a big deal because diseases caused by a single-point mutation like this are relatively uncommon. A company called Verve Therapeutics has designed a base editor to switch out a single letter in the stretch of DNA encoding for PCSK9 to essentially turn the gene off. Last year, they reported when they injected the therapy into the livers of monkeys it reduced their LDL levels by 60%. Human Clinical Trials StartedThe first human trial began this month with the first to receive the therapy a New Zealand volunteer. The plan is to treat 40 people who have an inherited condition called familial hypercholesterolemia (FH) which occurs in 1 in 250 and produces extremely high levels of LDL. Those with FH are at higher risk for heart disease. If successful the treatment can become a standard approach to dealing with FH and other high cholesterol risks. Stated Sekar Kathiresan, CEO of Verve, in a recent MIT Technology Review article, “If this works and is safe, this is the answer to heart attack—this is the cure.” The therapy is a one-and-done treatment unlike being on statins or taking monoclonal antibodies. It will make a permanent change to liver cells and stop them from producing the PCSK9 protein. The edits will pass on to the next generation of cells when they divide. That means that even if the therapy is initially expensive, the lifetime cost should prove to be comparable if not lower than current alternatives. The therapy is delivered to the liver cells in lipid nanoparticles, the same technology being used by mRNA Covid-19 vaccines. The pandemic has created manufacturing capacity for this type of therapeutic delivery which is helping to lower costs. A successful clinical trial doesn’t lead right away to adoption throughout the medical profession. It is likely there will be many more trials, and a number of years before Verve has enough data to convince regulators to approve the treatment for run-of-the-mill high cholesterol. If it turns out to become the new treatment standard, however, it will be one of the most transformational innovations in human healthcare to be seen in decades. Final Thoughts and Future PromiseBeyond the potential to cure heart disease, this news is an exciting milestone in the use of genetic engineering in clinical application. Current base editing technology is capable of tackling about 60% of single-point mutations associated with diseases and this could widen the scope for its use. Beam Therapeutics is another company working with base editing technology that is about to start human clinical trials designed to treat the genetic blood disorder sickle-cell anemia. It is using base editors to make multiple single letter changes for more complex genetic repairs. Then there is Wave Life Sciences that is experimenting with base editors to modify RNA rather than DNA to make it possible for transient changes to how genes are expressed rather than permanent alterations to the genome. Most excitingly, the researcher who first developed base editing, David Liu from the Broad Institute of MIT and Harvard, has continued innovating. In 2019, he and his colleagues outlined a new approach called prime editing in the journal Nature, which dramatically increased the scope of potential edits. Base and prime editing are being used by the team at CureHeart to tackle cardiomyopathies. You can read what I recently wrote about their work on this blog site. Like base editing, prime only breaks a single DNA strand, but in addition makes edits to individual letters or entire stretches of genetic sequences. It is believed that up to 89% of mutations associated with diseases in humans can be treated this way. |








