Two weeks ago, the New England Journal of Medicine published research and a trial for a malaria preventive developed and headed up by scientists at the Vaccine Research Center of the National Institue of Health (NIH) in Bethesda, Maryland. What they have done is synthesized a monoclonal antibody.
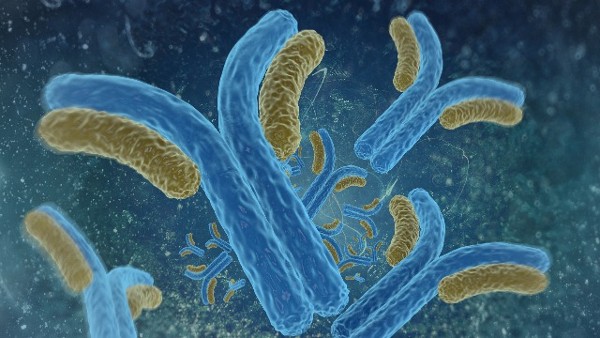
Monoclonal antibody therapy in the treatment of coronavirus has been in the news recently with the U.S. Food and Drug Administration authorizing emergency usage of some and reporting on the failure of others. They are experimental proteins made in a laboratory and designed to mimic natural proteins produced by the immune system to help fight off infection. In the case of malaria, NIH researchers identified a particular protein that the body produces for a short term when first infected with malaria parasites.
Malaria is spread by infected mosquitos. In 2019, 229 million cases were reported. The World Health Organization (WHO) 2019 statistics recorded 409,000 deaths that year with 274,000 of them being children under the age of five. The disease is the scourge of Africa which had 94% of cases and deaths. But half the planet’s population lives in areas where malaria is endemic.
Five parasites cause malaria. The two of greatest threat are Plasmodium Falciparum and Plasmodium Vivax. The former is dominant in Africa, Asia and Australasia. The latter is found more in the Americas.
When an infected mosquito bites a person, it takes between 10 and 15 days before the first symptoms appear. These begin as mild including fever, headaches and chills, which can be confused with less threatening infections. The confusion over the symptoms is what makes malaria a serious problem. If not treated immediately when the first symptoms present in the first 24 hours, adults can experience multi-organ failure, and children can develop severe anemia, respiratory distress, and fatal brain infection.
There are a number of vaccines being developed to reduce incidents of malaria. One of them is Mosquirix RTS, S/AS01, a recombinant malaria preventive containing proteins from the malaria parasite. It has demonstrated the ability to reduce the number of infections in children exposed to infected mosquitos with no evidence of recurrence.
The development of a monoclonal antibody, however, is a new avenue of approach that differs from a vaccine. Early success in a clinical trial involved 25 adult volunteers and 6 control participants. The monoclonal antibody introduced is called CIS43LS, and is a modified version of one that is naturally occurring in our bodies. It is called CIS43.
The work to develop CIS43LS involved scientists from the National Institute of Allergy and Infectious Diseases, Walter Reed Army Institute of Research, the Frederick National Laboratory for Cancer Research, all in Maryland, and the Schools of Medicine and Pharmaceutical Sciences at UC San Diego in California.
They isolated the naturally occurring antibody and recognized the role it played in identifying malaria infection. But CIS43 doesn’t have staying power. So the researchers modified it to extend its duration in the bloodstream. Two volunteer participants who received at the outset of the trial an infusion of CIS43LS underwent a controlled human malaria infection 36 weeks later. The monoclonal antibodies they received continued to protect them showing the long duration efficacy of treatment.
A larger clinical trial is now underway in Mali with ongoing research in the United States underway to determine minimal dosage requirements to completely protect people from being infected with the disease. In their conclusions, the researchers noted that “Among adults who had never had malaria infection or vaccination, administration of the long-acting monoclonal antibody CIS43LS prevented malaria after controlled infection.” The Mali trial will let them know if the same results can be achieved outside a laboratory in the wild.