May 20, 2015 – I have previously written about autoimmune diseases of which multiple sclerosis (MS) is one. Autoimmune diseases happen when our immune systems get confused and attack healthy living cells rather than infections. In MS the target cells form a protective layer around our central nervous system. The immune system attacks this layer which is known as the myelin sheath. This process of demyelination impacts the nerve cells (see comparison of normal and MS nerve cells below) eventually causing them to “short circuit.”
Over time MS scars the myelin leaving it sclerotic. In many cases MS patients experience remissions where, they can function normally, followed by relapses. Common symptoms include fatigue, loss of vision or double vision in one eye, muscle weakness, balance problems, and prickling or numbness in the skin. Living with MS, therefore, can be debilitating to a point where patients experiencing the worst symptoms become wheelchair bound and unable to function normally.
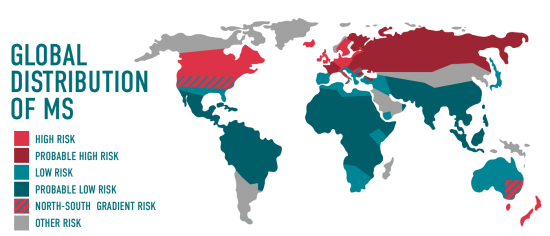
A striking aspect of MS is its geographic distribution. Almost exclusively north or south of the 37th parallels of latitude on either side of the equator with twice as many cases on the polar side of the line versus those in warmer latitudes. Highest density distribution can be found in Northern Europe, Russia, Canada, the northern United States, New Zealand and southeastern Australia. Average number of cases in these areas amounts to 30 incidents per 100,000 of population. Compare that to 5 in 100,000 in the tropics and in much of Asia. And another peculiarity of MS is that it appears to be a disease associated with people of northern European origin. Those of African, Japanese and Chinese descent have much lower incidents. Total number of people affected – an estimated 2.3 million worldwide. Why estimated? Because many people go about their lives with undiagnosed MS and some suspected cases of MS prove to be false with symptoms attributable to other conditions, some autoimmune in nature.
Diagnosing MS is not easy. The common tests such as magnetic resonance imaging to identify spinal cord scarring, lumbar punctures to check for spinal fluid abnormalities, and electrical stimulation tests are not always conclusive.
Identifying the autoimmune triggers that cause the body to turn on itself has been the pursuit of medical research teams around the world for more than a decade. One thing that has been noted, the T cells responsible for demyelination leading to scarring symptoms are found in both healthy and MS patients. The question then is why do these cells behave abnormally in some and not others.
Researchers at the Yale School of Medicine and Massachusetts Institute of Technology have discovered that the T cells in MS patients are producing inflammatory proteins not found in healthy patients. In the study the T cells of 45 patients were analyzed. Of these 23 were diagnosed with MS while the rest were free of the disease. In doing the comparison the researchers were able to isolate the MS protein trigger.
Proteins play an important role in the normal functioning of the cells in our bodies. They function as communicators, signaling cells for all kinds of function. Grow new bone here. Repair bruised tissue, and so on. In the case of proteins and the immune system, they signal T cells directing them to sites where there is infection or trauma. In MS patients, they produce this unique set of proteins that don’t repair the body but rather attack the sheath around healthy nerve tissue. The identification of these specific MS protein triggers means the potential to create specific protein blockers to stop the disease.
The researchers believe that what they have discovered for MS may also hold true for many other autoimmune diseases such as rheumatoid arthritis, ulcerative colitis, celiac , Crohn’s, angioedema, juvenile and Type 1 diabetes, drug hypersensitivity and others.
The Yale and MIT research paper appeared in the May 14th issue of Science Translational Medicine.