October 15, 2019 – Autoimmune diseases are tough to figure out when it comes to identifying which cells in our bodies turn against us. In the case of multiple sclerosis (MS), it is our own disease-fighting T-cells, the white blood cells in our bodies that end up attacking the nerve cells of our brain and spinal cord, eroding the nerve fibers’ protective myelin sheath.
T-cells, however, come in four varieties. There are natural killer T-cells, memory T-cells, CD8 cells that attack viruses and tumors, and CD4 cells, also known as helper T-cells. The latter, the so-called helper cells are turning out to be the causal agents for MS. And it isn’t all helper T-cells that are the culprits. It’s a group of cells designated TH17, and not all of them in that group, just some. Apparently a subset of TH17 cells bears a specific marker and are fast proliferators. The marker is a protein, labeled CXCR6, which can be found on the surface of a TH17 cell subgroup. The research shows that the TH17 cells bearing this protein damage nerve cells by turning on other proteins that stimulate inflammatory attacks including turning on other T-cells to join the assault.
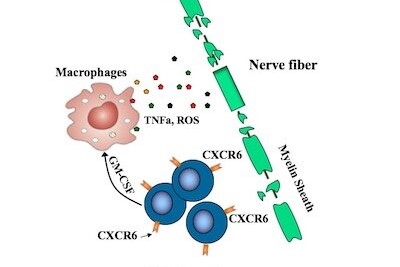
In a paper published last month in PNAS, The Proceedings of the National Academy of Sciences of the United States of America, a team of researchers from Children’s Hospital of Boston, describe potential treatments for MS targeting T-cells with the CXCR6 protein to deplete them while not impacting other immune defense mechanisms. Using monoclonal antibodies the researchers were successful in eliminating the harmful T-cells. They have patented their research and plan to commercialize the cure under a newly-formed company, Edelweiss Immune, Inc., in partnership with the Children’s Hospital.
Eileen Remold-O’Donnell, Department of Pediatrics, and Hematology/Oncology, at Harvard Medical School, and Lifei Hou, of the Program in Cellular and Molecular Medicine, Children’s Hospital and Department of Pediatrics, at Harvard, are lead authors in the research study. In an article published on the Medicalexpress.com site, Hous is quote stated, “Many drugs have been developed to treat autoimmune diseases, such as glucocorticoids and cytotoxic reagents…However, none selectively target pathogenic T-cells, and long-term use of immunosuppressive agents results in broad immunosuppression and compromised immune defenses.”
Remold-O’Donnell and Hou may have uncovered a means by which to deal with many other autoimmune diseases. Among these is Addison’s Disease made famous by President Kennedy, Celiac and Crohn’s both affecting the intestinal tract, Hemolytic Anemia attacking red blood cells, Juvenile and Type-1 Diabetes, Lupus, Psoriasis, Angioedema, Rheumatoid Arthritis, Ulcerative Colitis, and more.
If Hou and Remold-O’Donnell are correct in their findings. then their discovery of a specific protein could lead to finding the signature genes involved that influence the development of various helper T-cells and the potential to tackle other autoimmune diseases by revealing other proteins associated with these cells that trigger the autoimmune system to attack the host body in which they reside. The discovery of a cell surface protein marker, CXCR6, and treatment to deplete cells with the protein in finding a potential MS cure, therefore, bodes well for this line of medical research and for those suffering from autoimmune diseases globally.
How many people are we talking about? According to the American Autoimmune Related Disease Association (AARDA), there are more than 100 different autoimmune diseases affecting 5 to 10% of the world’s population, and in particular, women who are two to ten times more likely to suffer from an autoimmune disease than men. That means between 375 and 750 million people on the planet, the majority of them women, have an autoimmune disease. Of these, some 2.3 million suffer from MS, and most MS sufferers are found in more northerly climates which in itself, marks another peculiarity about this particular autoimmune disease.









