April 15, 2018 – When I left the apartment this morning to walk my dog Maya, Toronto was in the middle of a rare April two-day ice storm. Traveling anywhere was treacherous whether on two feet or using four wheels. The icy surfaces were a challenge to my osteoarthritic left knee. Fortunately, with a cane armed with a collapsible cleat, I was able to keep erect. But with every step, I became cognizant of just how disabling my osteoarthritis has become when I try to get around.
In Part 1 of this series on searching for a better knee, I talked about my recent visit to a Toronto clinic where I was assessed and provided with exercises and a plan to improve my mobility related to my osteoarthritic knee. It was reassuring not to be talking about scheduling knee replacement surgery, a procedure which I have been avoiding for many years.
In talking to the medical team at the clinic I mentioned regenerative medicine and the use of stem cells as an alternative to an artificial joint. It appeared that I knew more about this subject than the people advising me. In some respect, this seemed surprising to me. But then I realized, if the focus of this clinic’s efforts was on rehabilitation, why would it know about regenerative medicine related to knee joints. After all, the clinic was overseen by a team of orthopaedic surgeons. But not all orthopaedic surgeons are just thinking cut and replace these days when it comes to osteoarthritic knees.
On Friday I was sent a press release from PR Newswire featuring Kevin Plancher, an orthopaedic surgeon who in his practice is looking at both surgical and nonsurgical treatment of hip and knee joints. In the release, it describes the 50-year history of surgical joint replacement in the United States and notes that according to the Mayo Clinic, there are 1.5 times more Americans living with hip and knee replacement than there are living with heart failure. It went on to state that the outcomes for the vast majority have been good. But it also noted that some patients end up with multiple replacements or continue to suffer pain and limited mobility even after replacement.
Also in the release, Dr. Plancher describes the progress being made using growth factors and stem cell therapy. This technology is minimally invasive involving injections into an affected joint. The release talks about animal studies that have been showing promise by reversing the breakdown of cartilage and accelerating healing.
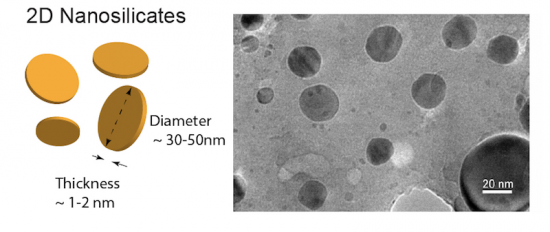
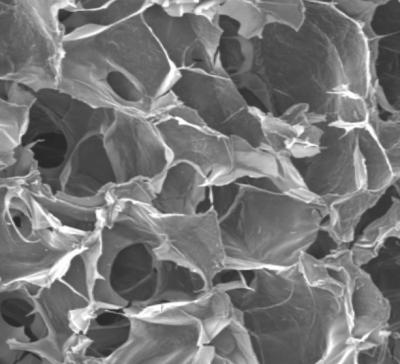
My own research into regenerative technologies indicates that there remain barriers to the use of stem cell therapy and it becoming an everyday procedure for restoring hips and knee joints. In the latest paper, I just read, however, researchers are introducing something new to regenerative therapy that could make the therapy viable. It is nanosilicates. What are nanosilicates? – a biodegradable synthetic material containing the mineral silica. When added to a bone grafting procedure, nanosilicate becomes a suitable scaffolding (like that seen in the picture below) that can be implanted into a joint to form the medium for regenerating bone or cartilage. Because nanosilicates are tiny they can put into a bio-ink containing a mixture of nanosilicate and stem cells that if injected into a damaged joint can begin the regenerative process.
In the latest paper on the subject of regenerative medicine that appears in the U.S. journal, Proceedings of the National Academy of Sciences (PNAS), researchers at Texas A&M University, Sloan Kettering Cancer Center, and Weill Cornell, have described applying nanoparticles to grow bone and cartilage from mesenchymal stem cells from a human donor.
The team, led by Akhilesh Gaharwar, describe the use of two-dimensional nanosilicates, 30 to 50 nanometers in diameter and 1 to 2 nanometers thick, to provide a scaffolding for bone and cartilage regeneration therapy. The work being done by this team is part of a new field called mineralomics and could prove to be the breakthrough advancement needed to make stem cell therapies viable as a future treatment for knee and hip osteoarthritis.
States Gaharwar, “Osteoarthritis progressively degrades cartilage and often specifically attacks the spaces between joints. Because these intra-articular spaces lack blood vessels, systemic delivery of morphogens and growth factors supporting cartilage matrix synthesis usually results in limited improvement. These nanoparticles could be delivered to this space to stimulate chondrocytes to synthesize new cartilage matrix.” Although the current study described in the PNAS-published paper involved human cells in vitro, Gaharwar believes that the technology could conceivably be used “to develop implantable scaffolds containing these nanomaterials to improve local tissue growth.”
So it appears that computational biology, genomics, and next-generation bioactive materials like nanosilicates, combined with human stem cells may prove to be the breakthrough that turns regenerative knee and hip joints into an alternative to surgically implanted joints. And because the stem cells will be harvested from the patients themselves, the body’s autoimmune systems will accept the material without a negative reaction.