At North Carolina State University, researchers have developed a smart stent that has regenerative therapeutic characteristics. If you are not familiar with stents, they are small metal prostheses that are inserted into blood vessels to open them up to improve vascular blood flow. The best analogy in terms of appearance is to think of the spring contained in your ballpoint pen.
Recently I had a cardiac ablation procedure that involved inserting a catheter through my femoral vein into my heart. The ablation would correct atrial fibrillation. an arrhythmia that happened after I was infected with COVID-19. During the catheter insertion, it nicked the vein wall creating a fistula, a small connection between my femoral vein and the neighbouring artery. The complication was discovered upon examination the morning after the procedure and one of the proposed solutions from the cardiology team was to put a stent in to block the hole which would stop the shunting of blood from the artery into the vein and a potential aneurysm.
It wasn’t the first time I had encountered stents. My daughter who was born with congenital heart disease in her last heart procedure had a stent containing a valve inserted into her pulmonary artery. She was born with an absent pulmonary valve among several other heart complications.
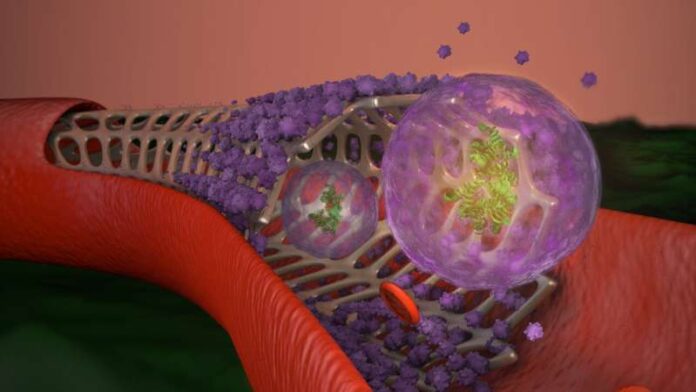
What makes the stent developed at North Carolina State different from any that I have read about or seen in the past is the fact that it uses exosomes from stem cells as a coating. The inventors call it the Exosome-Eluting stent or EES, the cell-derived material coating on the stent when implanted in a blood vessel counters the natural inflammatory response that automatically is triggered by our bodies to repair an injury. Stent-altered vessels often end up with post-procedure narrowing, a stenosis, caused by the body’s misguided attempts at healing. It’s a self-defeating proposition when trying to open blood vessels to support heart function when a narrowing occurs resulting from treatment.
The North Carolina team led by Ke Cheng, Professor in Regenerative Medicine and Biomedical Engineering, is using mesenchymal stem cell exosome secretions to camouflage the stent so that the body’s immune defenses cannot find it. The exosome-coating also promotes the growth of endothelial cells, the normal lining in blood vessels, which form over the stent.
Up to 60% of the coating is released within 48 hours after implantation which inhibits the effect of reactive oxygen species, unstable molecules produced by our cells that cause tissue damage at a post-operative injury site.
So far the studies have been done on rats to be followed by larger animals before human clinical trials. In a North Carolina State news release, Cheng states, “This bioactive stent promotes vascular healing and ischemic repair, and a patient wouldn’t need additional procedures for regenerative therapy after the stent is in place…The stent is the perfect carrier for exosomes, and the exosomes make the stent safer and more potent in tissue repair.”
A paper describing the EES appears in an April issue of Nature Biomedical Engineering.







[…] Cheng, who I wrote about two years ago because of his work using mesenchymal stem cells to create coatings to counteract the body’s immune and rejection response to implants like stents. In this, the professor’s latest project, he has developed an […]